Tomorrow starts my journey through CAR-T therapy in the hopes of once again putting my Mantle Cell Lymphoma (MCL) into remission and even possibly curing me of the disease.
Unlike my stem cell transplant 10 years ago, they won't be collecting stem cells. This time, they're collecting T-cells.
I'll get more into what CAR-T is later but, first, let's address the cost. My autologous stem cell transplant cost over $1,000,000. CAR-T will cost between $1,500,000 and 2,000,000, according to Richard T. Maziarz, MD, professor of medicine at Oregon Health & Science University’s Knight Cancer Institute.
"The total cost of care includes the cost of the drugs, its administration, and oftentimes inpatient care for toxic side-effects and that’s for an uncomplicated case. In the case of a Medicaid patient, it actually takes $2 million dollars before you break even."
Fortunately, we have a good health care plan as well as a secondary insurance. We're nearing our deductible already so the out of pocket costs will be a fraction of that price tag along with whatever it costs to get to and from the hospital each day after the extended stay.
Now, what is CAR-T Therapy?
The National Cancer Institute defines it as:
A type of treatment in which a patient's T cells (a type of immune system cell) are changed in the laboratory so they will attack cancer cells. T cells are taken from a patient’s blood. Then the gene for a special receptor that binds to a certain protein on the patient’s cancer cells is added in the laboratory. The special receptor is called a chimeric antigen receptor (CAR). Large numbers of the CAR T cells are grown in the laboratory and given to the patient by infusion. CAR T-cell therapy is being studied in the treatment of some types of cancer. Also called chimeric antigen receptor T-cell therapy.Watch this video from the Dana-Farber Cancer Institute for a visual interpretation:
Now that you know what it is, here's the process:
- Cell Collection/Induction: I'll have my cells collected on Thursday, May 30. That process could take an hour or up to six or seven hours, depending on the quantity needed (that quantity is determined by the lymphocytes present in my blood). They'll then take those cells to the lab and modify them. I can't really tell you what they do to them other than what you see in the video above. I think I skipped that day of chemistry...or biology...or whatever -istry or -ology you may learn about such things.
- Chemotherapy: I'll be admitted to the hospital on June 5. I'll begin a four-day regimen of chemo on June 6. I'll start with Cyclophosphamide on June 6 and then move to Fludarabine on June 7, June 8 and June 9.
- Consolidation: On June 10, I'll begin the day with a dose of Tocilizumab followed by consolidation, which is the CAR-T cell infusion.
- After the infusion, I will remain hospitalized for about a week and a half to two weeks to monitor the side effects.
- Daily Check-Ups: For 30 days after I am released from the hospital, I will return for blood counts and monitoring.
Although I'm certainly not looking forward to the hospital stay, I am in such a better place mentally than I was 10 years ago. I didn't know what was to come. I was scared and confused.
Now, I'm in a better place as far as understanding what I'm going to go through--having been there before--and I'll be better prepared to handle the long hospital stay.
During my stem cell transplant 10 years ago, I received five days of high-dose chemotherapy prior to the transplant. That basically knocked out my immune system. I have never felt worse in my life, mentally or physically.
This time around, the doctors have told me the chemo is not as intense but I do expect to have some side effects. The good news is I don't have anything to do and can sleep all day if I want to. My plans are to remain somewhat active both to prevent blood clots and to keep my mind busy.
Another reason for my optimism heading into CAR-T is I have a first-person account of the treatment.
About a month after I was diagnosed in 2009, my cousin reached out and told me her neighbor was diagnosed with the same disease. Paul almost followed my chemotherapy regimen to the Tee and also had a stem cell transplant.
He and his wife Amy actually visited me while I was in the hospital and Amy has become a close friend, although we have only met each other in person that one time.
We would often share the stories of our treatment and the progress we each recorded throughout that next year.
Unfortunately, Paul relapsed late last year and went through CAR-T therapy at Cleveland Clinic in December.
The good news for me is I now have a personal connection to the therapy I'm going to endure. I have talked with Amy quite a bit about what Paul went through and the side effects he endured.
With her permission, I'm going to share some of Amy's comments.
My first conversation with Amy about Paul's CAR-T treatment occurred on Dec. 12. She provided some of the statistics:
"It’s got an 85% chance that it won’t kill him, 73% chance that he has a response, and if so, a 50% chance that it will be curative."That's really the key with CAR-T therapy, that they talk about a cure rather than a remission and that's what we're hoping here.
Our next conversation was on April 23 when I shared the news of my relapse.
I loved this comment from her:
"CAR-T cell is like crazy nano science."It really is. Think about...they're taking diseased cells and training them to kill other diseased cells, reinfusing them into the patient and letting them do their thing. It's crazy.
Early in the discussions of how we'd treat my relapse, I shared with Amy the idea we may go with an Allogeneic transplant or with CAR-T. She responded:
"I also wanted to tell you allo is still on the table for Paul should he relapse, but the word cure is associated with CAR-T, so who knows if it'll become necessary. I asked him this morning if he feels it was worth it. He said yes. He's still tired, but we can't say if that's CAR-T or the blood loss/kidney damage. Other than that, he's pretty good."Paul had some other issues unrelated to the CAR-T therapy, so some of his side effects likely won't occur with my therapy.
Now, on to Paul's adventures in the hospital...and this is where I get both excited and a bit nervous.
Paul's infusion took about 15 minutes and for five days or so following that consolidation all went well.
"Then he got a little whacky for a few days," Amy said. "Got some fever. Had some (blood pressure) changes. Spent a day in ICU because of that. They hooked him up to nonstop fluids (which they couldn't do on the floor). He regained his BP stability and they shipped him back to the floor. Then they just watched him for another week and a half or so. The main thing is they wanted him to be mentally clear."That mental clarity is one of the biggest concerns with CAR-T therapy.
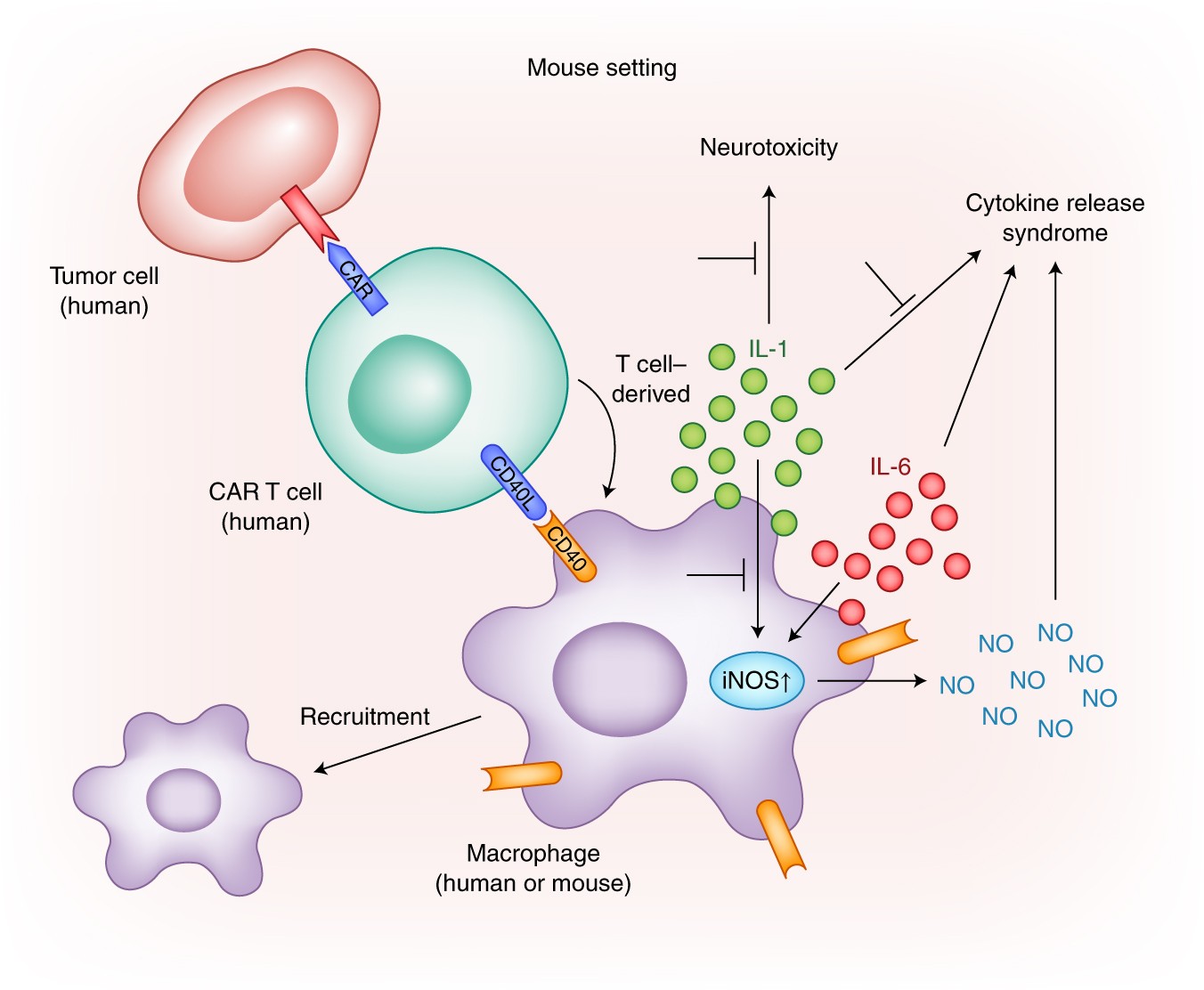 |
| Modeling Cytokine Release Syndrome |
The Cleveland Clinic describes CRS as an effect "similar to flu-like symptoms (headache; fever; chills; severe nausea, vomiting, diarrhea; severe muscle or joint pain), shortness of breath, low blood pressure and fast heart rate. These symptoms are mild in most patients but can be serious and life-threatening."
The Clinic also has observed neurologic events in some patients.
"Neurologic events include encephalopathy (brain disease, injury, malfunction), confusion, aphasia (difficulty understand or speaking), drowsiness, agitation, seizures, loss of balance and altered consciousness."Amy witnessed that confusion in Paul and other patients.
"He seemed a little far away, and when I came in the room, he said he had a dream that he had won $23 million in the lotto," Amy said. "I said, 'oh wow, too bad it's just a dream.' He said, 'Well I gave it all to you. You can have every penny.' It seemed to me like he wasn't just describing a dream. He said he woke up four minutes before he was supposed to and that he'd need to make up the time during his next nap; that sort of thing. He went to the dayroom in his boxers with his gown, something he wouldn't normally do."The confusion was out of the ordinary for Paul.
"I noticed it, too, when Paul would order his food. He was very adament (not like him)... the guy would say chicken or pot roast? and he'd say turkey."Paulette likely will need to be with me during those few days following infusion. Amy stayed with Paul.
"It was kind of a lonely feeling, wondering if he'd come out of it," she said. "I slept in the room with him. He also wanted to get out of bed all the time and they put the alarm on, so then he got agitated by it going off."And Amy's warning to me:
"I’m just saying that if you think the night time is it where you close your eyes and take long rest, you might be surprised," she said. "Paul had a hard time staying in bed. The nurses told us about it. Some people who like to strip out of clothes and be naked, and one guy did tai chi for several days. Paul didn’t really get all the way naked but he did rip his shirt off quite a few times. I think because of feeling hot really."I hope there aren't cameras on the floor. Those are some pictures of me nobody will need to see!
In order to gauge my mental acuity before, during and after the transplant, the doctors will start with a mental assessment.
They'll use that baseline to compare where I'm at when symptomatic and later.
"Something interesting is that intelligent people kind of tend to trick the nurses and doctors, according to his oncologist," Amy said. "So he could pass the assessment because he could do the math of subtracting seven from 100 multiple times, but the little things is how I noticed that it wasn’t totally mentally himself, like obsessing over what he would order for his lunch and stuff like that. So they gave a lot more credence to what I was noticing rather than what he was reporting because Dr. Dean felt pretty sure he was masking and then when he realized he had said something off the intelligent side of him would kick in then he would sort of cover for it and laugh it off as though he had been incredibly funny by intent, but I told Dr. Dean that’s not the way he would normally be funny, so it was more like weird humor."One thing my doctor told me about the CRS is the doctors and nurses are much better at pre-treating the symptoms using Tocilizumab, which I'll get with my infusion.
They have learned about the side effects and the drug seems to help curb those symptoms.
While some of this is a bit scary the good news is Amy said Paul could have gone back to work after basically two months--the month of the CAR-T and a month of recovery. As a professor, he took off the whole semester so he didn't have to go back to work.
I'm hoping to be ready to go back to work when fall sports start in mid-August.
Hearing from Amy about Paul's experience certainly has calmed my nerves and leaves me hopeful that I'll be back to "normal" at some point this summer. I'm not making any plans--as I don't want to be disappointed--but I am encouraged by Paul's progress.
I'm also encouraged by the story of Emily Whitehead, who as an infant fought Acute Lymphoblastic Leukemia (ALL), for almost all of her first year of life.
"In the experimental treatment, Emily's T cells would be collected from her blood, then reprogrammed in a lab to recognize and attach to a protein called CD19 that is found only on the surface of B cells. After this reengineering, the cells are called chimeric antigen receptor T cells. When the reengineered cells are put back into the patient, they disperse throughout the body to find and kill cancerous B cells."Emily became the first pediatric patient to be enrolled in a CAR-T trial.
She is now 12-years old and recently won an award from Time Magazine for an essay she wrote about her doctor.
"Dr. June saved my life and had a huge impact on my family. Without him, I wouldn't be here today writing this — and my parents and I wouldn't be helping other kids beat cancer," Emily wrote in her Time tribute. "Dr. June is my hero."Emily did it. Paul did it.
I can do it too.


No comments:
Post a Comment