I have now referenced CAR-T therapy several times. Here's a bit of a primer on what it is and how it works.
What is CAR T-cell therapy?
When the immune system is functioning normally, immune cells move around the body looking for things that don’t belong, like bacteria and viruses. These immune cells search for invaders using “receptors,” which can be thought of as antennae or feelers. When receptors find invaders in the body, special immune cells come in to destroy them. These special cells are called cytotoxic T cells.Unfortunately, cancer cells are often able to hide from immune cells, which is why the cancer cells can grow out of control. Immunotherapy is a cancer treatment intended to make the body’s immune system able to detect and destroy cancer cells. Immune checkpoint inhibitors have been a successful immunotherapy approach because it pushes the immune system into high gear to fight cancer.
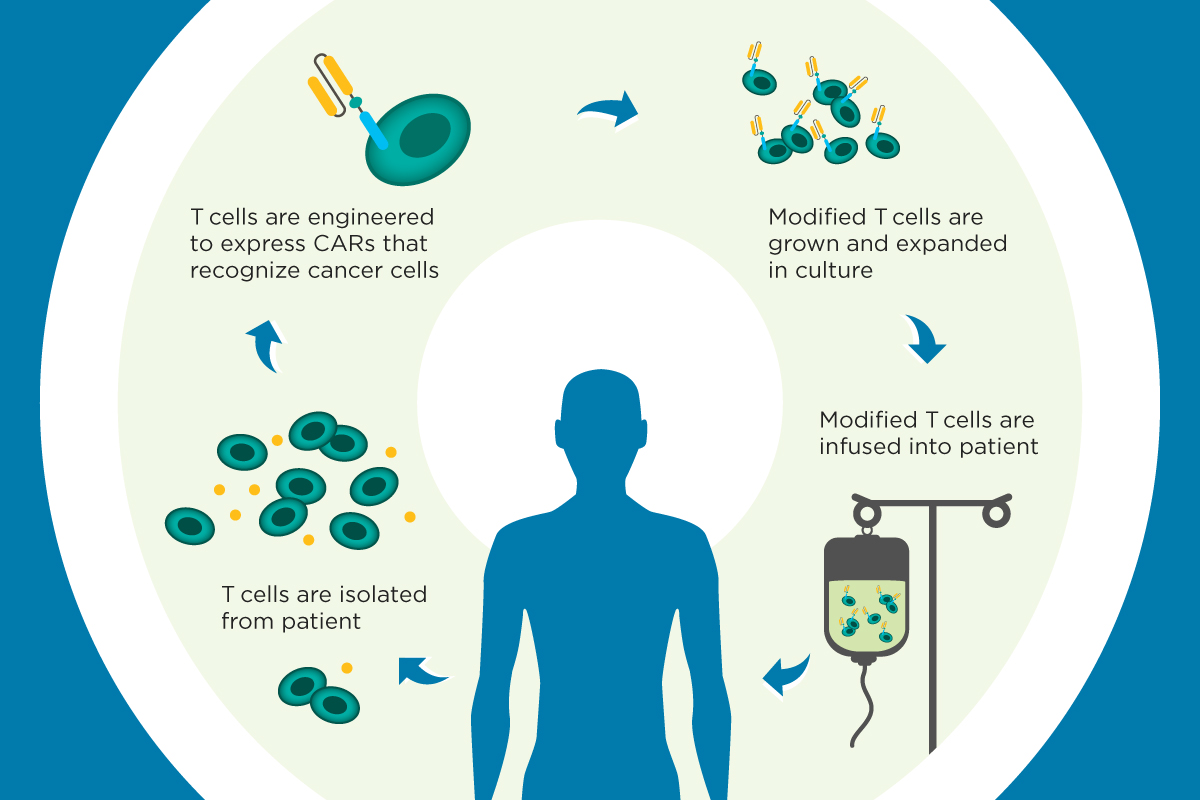
CAR T-cell therapy, however, is different. It is a type of immunotherapy called “adoptive cell immunotherapy.” As ASCO President Bruce E. Johnson, MD, FASCO, describes it, this technique “allows clinicians to genetically reprogram patients’ own immune cells to find and attack cancer cells throughout the body.”
In CAR T-cell therapy, a person’s T cells are removed and taken to a laboratory. The T cells are genetically changed so they will attack cancer cells. These CAR T cells are grown in large numbers and then injected into the patient. One of the remarkable things about this treatment is that it is a “living therapy.” CAR T cells typically have to be injected only once, because they go on to multiply in the body. CAR T cells continue fighting the cancer in the patient’s body, and their effectiveness may even grow over time.
What successes have there been with CAR T-cell therapy?
Here are 3 recent examples of the potential that adoptive cell immunotherapy brings to cancer treatment.
Childhood acute lymphoblastic leukemia (ALL).
Nearly 3 of every 4 children with leukemia are diagnosed with a type called ALL. Treatment for this form of leukemia has improved greatly over the years, so 90% of children are still alive 5 years after their diagnosis. But in about 600 children and young adults with ALL in the United States every year, treatment doesn’t stop the disease from returning. If this happens, survival time is usually measured in just weeks to months.In a clinical trial with children and young adults with ALL that had not been stopped by standard treatment, a CAR T-cell therapy called tisagenlecleucel (Kymriah) sent the cancer into remission in 52 of the 63 patients. In 3 out of every 4 patients, the ALL still had not come back after 6 months. Based on the results of this study, in August 2017, the U.S. Food and Drug Administration (FDA) approved tisagenlecleucel to treat children and young adults with recurrent ALL.
Non-Hodgkin lymphoma.
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma and is quite aggressive. Many people can be successfully treated with a combination of chemotherapy and rituximab (Rituxan), a targeted therapy. However, these types of lymphomas can sometimes worsen during treatment, called “refractory lymphoma,” or they can come back after treatment, called “recurrent lymphoma.” In these cases, CAR T cells may be an effective treatment option.A clinical trial used tisagenlecleucel to treat people with DLBCL that had worsened after at least 2 previous treatments. The lymphoma went into remission in 43% of the patients in the study. At 6 months after receiving the CAR T-cell therapy, the lymphoma had still not come back in nearly 80% of the patients.
Another study used a different CAR T-cell therapy to treat refractory lymphoma or recurrent lymphoma. In this study, people had DLBCL, primary mediastinal large B-cell lymphoma (an aggressive form of DLBCL that forms in the chest), or transformed follicular lymphoma (a slow-growing subtype of NHL that has turned into DLBCL). The CAR T-cell therapy in this study was called axicabtagene ciloleucel (Yescarta). The immunotherapy slowed or stopped cancer growth in 82% of the patients, and the cancer completely disappeared in more than half (54%). After nearly 9 months, about 40% of the patients still had no signs of cancer. In October 2017, the FDA approved axicabtagene ciloleucel for the treatment of DLBCL that has not been stopped by 2 or more previous treatments.
Multiple Myeloma.
Multiple myeloma is a blood cancer that involves the plasma cells in the bone marrow. Plasma cells play an important role in the body’s immune system. Multiple myeloma is an incurable disease, and only about one-half of people live 5 years after a diagnosis.Results from an early clinical trial presented at the 2017 ASCO Annual Meeting showed that a type of CAR T-cell therapy that targets a biomarker known as B-cell maturation antigen (BCMA) can stop multiple myeloma in its tracks. This study included 35 people with multiple myeloma that had come back after treatment, called relapsed or recurrent, or was resistant to treatment, called refractory. Of those 35, 33 patients (94%) had their multiple myeloma go into remission within 2 months of receiving the BCMA CAR T cells.
Are there risks involved with CAR T-cell therapy?
This new cancer treatment approach is powerful and does come with serious risks that need to be considered before starting therapy. In particular, possible side effects include cytokine release syndrome (CRS) and neurologic problems.CRS
CRS is caused when CAR T cells produce a storm of inflammatory molecules. CRS can cause a long-lasting fever, low blood pressure, difficulty breathing, and problems with different organs. Severe CRS can be a life-threatening problem that requires intensive medical care, including the use of a ventilator, drugs to increase blood pressure, and seizure medicines. In August 2017, the FDA approved tocilizumab (Actemra) to stop and, in most cases, cure CRS.Neurologic problems
CAR T-cell therapy can also cause neurologic problems. These may include problems remembering words, difficulty speaking, being less alert, delirium, hallucinations, seizures, and coma. In many patients, these problems go away on their own in a few days, but some have died from these problems.In people with ALL, there were many serious side effects from the CAR T-cell therapy. Nearly half of the patients developed severe CRS. Another 15% of patients had neurologic problems. In most patients, these side effects went away within a few days without long-term consequences, and there were no deaths caused by side effects.
For both non-Hodgkin lymphoma treatments, serious side effects were seen in the study participants. Around 1 in 4 patients taking tisagenlecleucel experienced severe CRS, and around 1 in 10 had neurological problems. Axicabtagene ciloleucel caused severe CRS in around 1 out of every 10 patients, and nearly 3 out of every 10 had neurological problems.
Among the patients treated for multiple myeloma, only 2 patients experienced severe CRS, and none experienced neurologic complications from BCMA CAR T-cell therapy.
Source
No comments:
Post a Comment